Proctologists and colorectal surgeons are specialists a general doctor may recommend to patients experiencing symptoms or issues related to the lower digestive tract. This could be in the form of persistent rectal pain, bleeding, and irregular bowel movements.
What’s the difference between these two professions? None. They can be used interchangeably, although colorectal surgeons are preferred by doctors today who specialise in colon and rectum.
This article discusses these roles, detailing the evolution from proctologist to colorectal surgeon and explaining the conditions these specialists treat.
What Is A Proctologist?
The term proctologist originates from a time when the medical community began recognising the need for a speciality focused on diseases of the colon, rectum, and anus.
Back in 1835, the field of proctology was emerging in response to a gap in medical care. Many doctors were reluctant to treat these conditions, leading patients to seek help from less reputable sources, often resulting in mistreatment.
To address this, a group of doctors established the speciality of proctology, aiming to provide professional and effective care for these intimate and complex conditions.
Historically, a proctologist was a doctor who specialised in the rectum, anus, and sigmoid colon. Their focus was narrow, primarily dealing with diseases confined to the lower portion of the digestive system.
Common conditions treated by proctologists included haemorrhoids, anal fissures, fistulas, and chronic constipation issues.
The term “proctologist” emphasises a specialist’s expertise in diagnosing and treating disorders in the proctology area, using both medical and surgical methods.
When Did The Title Colorectal Surgeon Begin?
The transition from the term proctologist to colorectal surgeon was motivated by the need for clarity and precision in the scope of this medical speciality.
The term “proctologist” comes from the Greek word “proktos,” meaning anus, which inaccurately suggested that these specialists focused solely on the anal region. This narrow interpretation did not reflect the wide range of conditions treated by these doctors, including diseases of the colon, rectum, anus, and pelvic floor.
To better represent the comprehensive nature of their work, the designation evolved to “colon and rectal surgeon”, or colorectal surgeon in short, a term encompassing the full breadth of their expertise.
Colorectal surgeons in Singapore are professionals who have completed extensive education and training in both general surgery and specialised colorectal surgery.
They handle a wide variety of conditions, from benign diseases like haemorrhoids to more serious conditions such as colorectal cancer, using both surgical and non-surgical treatments.
Colorectal Surgeon Training And Qualifications
Becoming a colorectal surgeon in Singapore involves rigorous training and education. Initially, one must earn a medical degree over 5 to 6 years, followed by postgraduate medical training in various disciplines to secure general medical registration with the Singapore Medical Council.
Aspiring colorectal surgeons then undertake specialist general surgery training for around 5-6 years, gaining certification from professional bodies. Subsequently, they undergo advanced surgical training in colorectal surgery under expert supervision, including local and international opportunities.
To practise, they must pass exams and fulfil the Specialist Accreditation Board’s requirements, being registered as specialists in general surgery with a subspecialty in colorectal surgery.
Continuous professional development through Continuing Medical Education is essential to stay abreast of advancements. Singapore’s strict standards ensure its colorectal surgeons are highly qualified, often holding affiliations with prominent medical associations to enhance their expertise further.
Conditions Proctologists Or Colorectal Surgeons Treat And Manage

Colorectal surgeons are equipped with the expertise to diagnose, manage, and treat these conditions through a combination of medical treatments and surgical procedures. Their specialised training allows them to help patients suffering from these often complex and sensitive health issues.
- Haemorrhoids: Enlarged veins in the rectal region, leading to discomfort, itchiness, and bleeding.
- Anal Fissures: Minor lacerations in the anal skin, causing pain and bleeding with bowel movements.
- Anal Fistulas: Unusual pathways connecting the anal canal to the skin surrounding the anus, typically arising from infection.
- Anal Abscesses: Infections filled with pus located near the anus or rectum.
- Diverticulitis: Swelling or infection of tiny sacs (diverticula) in the colon walls.
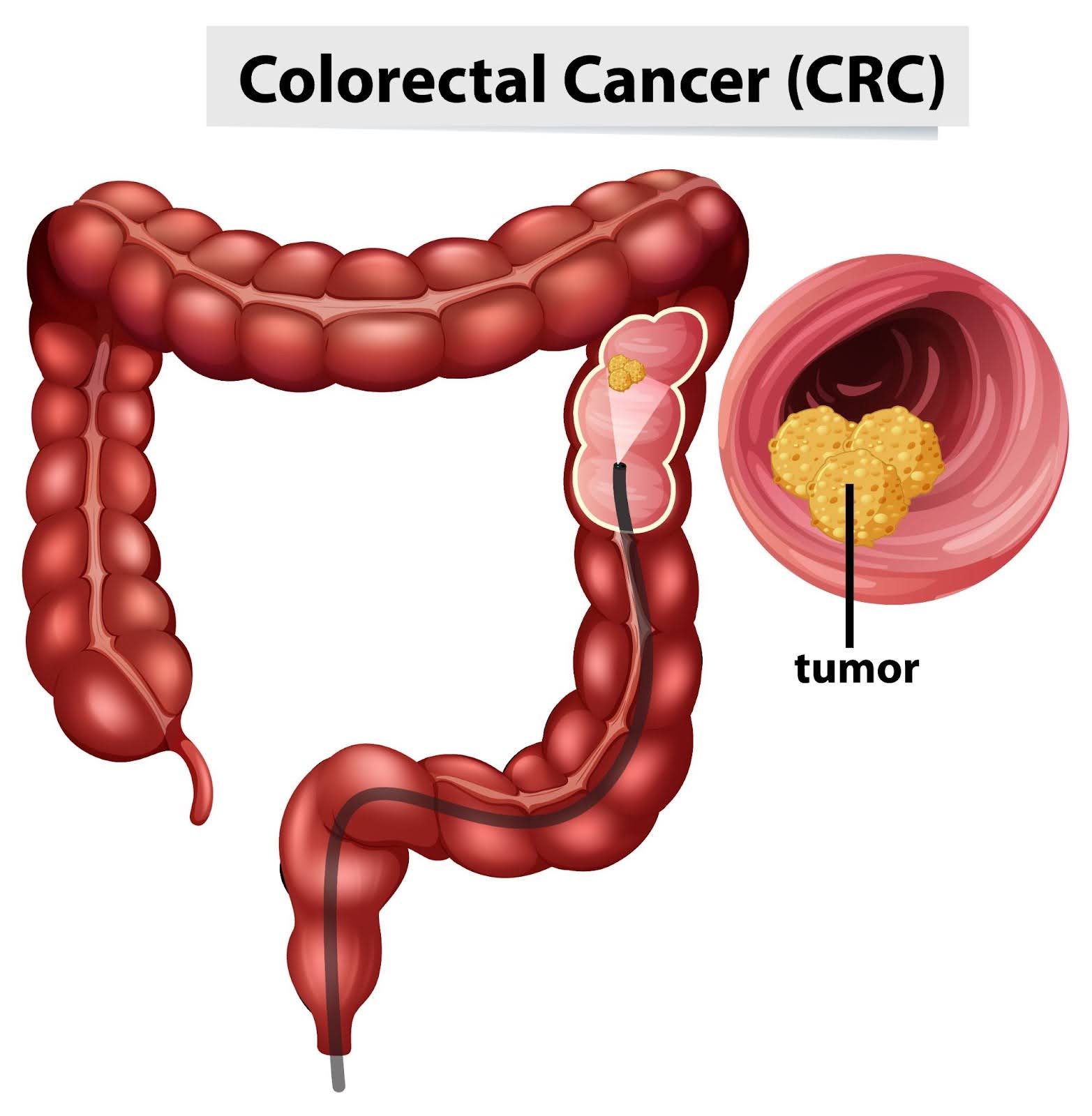
- Colorectal Cancer: Tumours found within the colon or rectum, necessitating specialised surgical procedures.
- Crohn’s Disease: A variant of inflammatory bowel disease impacting any segment of the gastrointestinal tract, including the colon.
- Ulcerative Colitis: A chronic inflammatory bowel disease resulting in prolonged inflammation and ulcers within the colon and rectum.
- Pilonidal Disease: Persistent skin infection situated in the buttocks’ crease adjacent to the tailbone.
- Rectal Prolapse: The descent of the rectum, protruding through the anus.
- Faecal Incontinence: The inability to retain bowel contents leads to unintended stool leakage.
- Constipation: Persistent difficulty in stool passage, often needing clinical management.
- Rectocele: Protrusion of the rectum’s front wall into the vagina’s back wall.
- Colon Polyps: Lesions on the colon’s inner surface, potentially pre-cancerous.
- Pelvic Floor Dysfunction: Disorders affecting the pelvic floor muscles’ coordination and relaxation, necessary for bowel movements.
- Pruritus Ani: Persistent anal itching.
- Lynch Syndrome and Other Genetic Colon Cancer Syndromes: Genetic disorders elevate the risk for colon cancer and additional cancers.
Medical Procedures Colorectal Surgeons Perform

Colorectal surgeons perform a wide array of procedures to diagnose, manage, and treat various diseases, ranging from benign to life-threatening. People don’t know that they also do diagnostic evaluations or screenings apart from surgeries.
Colonoscopy
This is the most comprehensive screening tool for colorectal cancer. It is necessary to visually examine the entire colon and rectum. This allows the surgeon to check for any abnormal growths or polyps.
Colonoscopy is recommended as a routine screening tool starting at age 50, but earlier or more frequent screenings may be advised for those with a higher risk.
Flexible Sigmoidoscopy
The procedure also involves using a flexible tube to check the rectum and the lower part of the colon. While less invasive than a full colonoscopy, it does not allow the entire colon to be examined, so its use as a screening tool may be limited to specific circumstances.
CT Colonography (Virtual Colonoscopy)
This imaging procedure uses CT scans to create detailed images of the colon and rectum. It is recommended as a less invasive alternative to traditional colonoscopy for patients who are medically unable to undergo the latter.
Minimally Invasive Surgery
Minimally invasive surgery, including laparoscopic and robotic-assisted techniques, represents a significant advancement in colorectal surgery. These approaches involve making several small incisions through which specialised instruments and a camera are inserted to perform the surgery.
The benefits of minimally invasive surgery are manifold: reduced pain and scarring, shorter hospital stays, and faster recovery times compared to traditional open surgery.
Laparoscopic surgery is widely used for a variety of colorectal conditions, including the removal of cancerous growths, the repair of hernias, and the treatment of diverticulitis.
Major Resection Surgery
For advanced cases of colorectal cancer and other severe conditions, major resection surgery may be necessary. This surgery is done to remove the affected portion of the colon or rectum and possibly nearby lymph nodes.
Resection procedures are critical in the management of colorectal cancer, ensuring the complete excision of cancerous tissues while striving to preserve as much of the healthy bowel as possible.
Techniques vary depending on the location and extent of the disease, including total colectomy, partial colectomy, and low anterior resection.
Anorectal Surgery
Anorectal surgery addresses conditions affecting the anal region and lower rectum, such as haemorrhoids, anal fissures, and fistulas. These are common problems that can cause significant discomfort and impact the quality of life.
Hemorrhoidectomy, for instance, involves the removal of haemorrhoids, offering relief from bleeding, irritation, and swelling. Surgery for anal fissures typically aims to relax the anal sphincter muscle, reducing pain and facilitating healing.
For anal fistulas, various procedures can be performed to close the fistula tract and prevent recurrent infections. Anorectal surgery often benefits from minimally invasive techniques, reducing recovery time and improving patient comfort.
Conclusion About Proctologist Vs Colorectal Surgeon
Seek a colorectal surgeon when experiencing symptoms related to the colon, rectum, or anus or for routine screenings to prevent colorectal cancer.
Consider scheduling a visit to Advanced Colorectal and General Surgery. We offer same-day colonoscopy, allowing you to get a consultation and get fast results. Our resident colorectal specialist, Dr QM Leong, provides an honest diagnosis and compassionate care.
Frequently Asked Questions About Proctologist Vs Colorectal Surgeon
What Can I Expect During My First Visit To A Colorectal Surgeon?
During your first visit, the colorectal surgeon will review your medical history, perform a physical examination, and discuss your symptoms. Diagnostic tests, such as blood tests, colonoscopy, or imaging studies, may be recommended to understand your symptoms’ cause and create a suitable treatment plan.
Is Colorectal Surgery Safe?
Colorectal surgery is generally safe when performed by an experienced and qualified surgeon. As with any surgical procedure, there are risks involved, but advancements in surgical techniques, including minimally invasive surgery, have significantly reduced these risks and improved recovery times.
How Long Is The Recovery After Colorectal Surgery?
Recovery time varies depending on the type of surgery performed, the individual’s overall health, and the presence of any complications. Minimally invasive surgeries tend to have shorter recovery times, often allowing patients to return to normal activities within a few weeks. Your surgeon will provide specific guidance based on your situation.
How Do I Prepare For A Colonoscopy Or Other Diagnostic Procedures?
Preparation for a colonoscopy typically involves following a special diet the day before the procedure and taking a laxative to empty the colon. Your colorectal surgeon will provide detailed instructions on how to prepare, including dietary restrictions and any necessary medication adjustments.