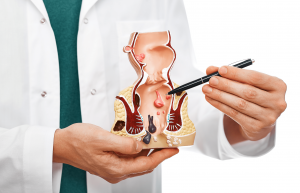
Rectal pain and pressure can be uncomfortable and sometimes alarming symptoms. These sensations can stem from a variety of causes, ranging from mild and manageable conditions to more severe health issues.
This article explores the potential causes, their symptoms, and available treatments. It also tackles the diagnostic procedures to determine the exact cause of rectal pressure and pain and for effective pain relief.
Table of Contents
Toggle1. Haemorrhoids
Haemorrhoids can cause discomfort, itching, pain, bleeding, and pain when sitting and during bowel movements. Haemorrhoids are swollen veins that may be located internally (inside the rectum) or externally (under the skin around the anus). External haemorrhoids might produce more pain and swelling in the area of the anus.
Haemorrhoids Treatments
Treatment for haemorrhoids often includes over-the-counter creams or suppositories, warm baths, and keeping the anal area clean. Dietary changes, like increasing fibre intake, can help prevent constipation and straining, which can exacerbate haemorrhoids.
In severe cases, procedures like rubber band ligation, sclerotherapy, or surgery may be recommended.
2. Anal Fissures
An anal fissure is a small tear in the thin, moist tissue lining the anus. Fissures can cause pain, especially during bowel movements, and bleeding. The pain is often described as sharp and severe. People may also experience spasms in the ring of muscle at the end of the anus (anal sphincter).
Anal Fissure Treatments
Most anal fissures heal with home treatments, such as warm baths, increased fibre intake, and over-the-counter pain relievers.
Applying topical anaesthetics to numb the area can help relieve pain during bowel movements. In cases where fissures do not heal with home treatment, prescription creams or surgery may be required.
3. Proctitis
Proctitis is inflammation of the lining of the rectum. It can cause symptoms such as a frequent or continuous feeling of needing to have a bowel movement, rectal bleeding, mucus in the stool, rectal pain, and pain on the left side of the abdomen.
People with proctitis might also experience a sensation of fullness in the rectum.
Proctitis Treatments
Treatment of proctitis depends on the cause. If an infection causes it, antibiotics or antiviral medications may be prescribed. For inflammatory causes, such as inflammatory bowel disease, medications to reduce inflammation might be used. Dietary changes and symptom management, like sitz baths, can also help.
4. Constipation

Constipation or difficulty passing hard or lumpy stools can cause rectal pain. Due to the straining during bowel movements, a sensation of incomplete evacuation, and discomfort or pain in the abdomen and rectum.
Constipation Treatments
Treatment often includes lifestyle changes like increasing fibre intake, drinking more fluids, and regular exercise. You can take over-the-counter laxatives for short-term relief. For chronic constipation, a healthcare provider might recommend prescription medications or, in rare cases, surgery.
5. Abscesses
An anal or rectal abscess, which is a painful collection of pus, may cause severe pain, swelling, redness, and tenderness in the area around the anus or rectum. Other symptoms can include fever, fatigue, and a noticeable lump or mass at the anal opening. The pain usually intensifies during bowel movements.
Abscess Treatments
Treatment usually involves surgical drainage of the abscess, which is often done under local anaesthesia. Antibiotics may be prescribed if an infection is present. Pain management and keeping the area clean are important aspects of post-procedure care.
6. Inflammatory Bowel Disease (IBD)
Crohn’s disease and ulcerative colitis cause chronic inflammation of the digestive tract and can lead to rectal pressure or pain.
Among the other common symptoms of these Inflammatory Bowel Diseases include diarrhoea, abdominal pain, blood in the stool, weight loss, and fatigue. The severity of symptoms can vary and often fluctuates with periods of remission and flare-ups.
IBD Treatments
The goal of the treatment for IBD is to reduce inflammation and suppress the immune system. Doctors may recommend corticosteroids, immunomodulators, and biologics.
Dietary changes and nutritional support may also be necessary. In severe cases, surgery to remove a damaged portion of the digestive tract might be required.
7. Rectal Prolapse
Rectal prolapse involves the rectum stretching and protruding from the anus. It can cause symptoms like a feeling of a bulge or lump in the anus, discomfort or pain during bowel movements, mucus or blood discharge from the protruding tissue, and incontinence (difficulty controlling bowel movements).
Rectal Prolapse Treatments
The treatment for rectal prolapse may include lifestyle changes, pelvic floor exercises, or stool softeners to reduce straining. In more severe cases, surgery may be necessary to repair the prolapse.
Several surgical options are available, and the choice depends on the patient’s overall health, age, and the severity of the prolapse.
8. Colorectal Cancer
Colorectal cancer patients often experience changes in bowel habits (like diarrhoea or constipation), rectal bleeding or blood in the stool, persistent abdominal discomfort (like cramps, gas, or pain), a feeling that the bowel doesn’t empty completely, weakness or fatigue, and unexplained weight loss.
In the early stages, colorectal cancer might not cause any symptoms.
Colon Cancer Treatments
Depending on the stage of colon cancer, treatments may include surgery (to remove cancer), radiation therapy, chemotherapy and targeted drug therapy. Early detection significantly improves the prognosis.
9. Sciatica

Sciatica can cause rectal pain and pressure. While sciatica pain is usually felt in the lower back and legs, it can sometimes affect the pelvic area and cause discomfort in regions such as the rectum. This is because the nerve pain or nerve compression causing sciatica can sometimes extend to these areas.
However, rectal pressure is not the most common symptom of sciatica. Most people with this condition experience lower back pain, hip pain, and burning or tingling down the leg. It usually affects only one side of the body.
Sciatica Treatments
Treatment options include physical therapy, and medications (like pain relievers, anti-inflammatories, and muscle relaxants), and, in severe cases, surgery. Home remedies like heat/ice therapy and exercises can also provide relief.
10. Endometriosis
This condition happens when a person’s uterine lining grows outside the uterus. Endometriosis can cause rectal pain in women if it involves the bowel or is located near the rectum.
More common symptoms include painful periods, pain during intercourse, urinating, and bowel movements. It can also accompany excessive bleeding and infertility.
Endometriosis Treatments
Treatment includes pain medications, hormone therapy (like contraceptives or other hormonal treatments), and surgery (to remove endometrial tissue). The choice of treatment depends on the severity of symptoms and whether the woman wishes to become pregnant.
11. Fibroids
Uterine fibroids are benign tumours that develop in the uterus. Large fibroids can cause rectal pain by putting pressure on the rectum.
However, the primary symptoms are heavy menstrual bleeding, prolonged periods, pelvic pressure or pain, frequent urination, difficulty emptying the bladder, constipation, and backache or leg pains.
Fibroid Treatments
Treatment options include medications (to regulate menstrual cycle or shrink fibroids), noninvasive procedures (like MRI-guided focused ultrasound surgery), minimally invasive procedures (like uterine artery embolisation), and traditional surgical procedures (like myomectomy or hysterectomy).
Diagnosing The Cause Of Rectal Pressure And Pain

Determining the exact cause of rectal pain and pressure can be challenging, as several different conditions can produce similar symptoms. However, certain steps and considerations can help narrow down the potential causes.
Note The Specific Symptoms And Their Patterns
Keep track of your symptoms, including the nature of the pain (sharp, dull, throbbing), its duration, any triggers, and associated symptoms like bleeding, changes in bowel habits, or weight loss. Symptoms can often provide clues about the underlying condition.
Consult A Healthcare Professional
This is the most important step. A healthcare provider, such as a colorectal specialist, can conduct a thorough examination and ask detailed questions about your medical history and symptoms.
Based on the initial evaluation, your doctor may recommend tests such as:
- Digital Rectal Exam (DRE): The doctor examines the rectum manually to check for abnormalities.
- Anoscopy or Proctoscopy: Instruments are used to visualise the inside of the rectum.
- Colonoscopy Screening: For a more extensive examination of the entire colon and rectum, the doctor may recommend a colonoscopy.
- Imaging Tests: Ultrasound, MRI, or CT scans can provide detailed images of the rectum and surrounding areas.
- Stool Tests: This is conducted to check for blood or signs of infection in the stool sample.
- Blood Tests: This is necessary to look for signs of infection, inflammation, or other markers that might indicate a specific condition.
Consider Your Medical History
Pre-existing conditions such as inflammatory bowel disease, endometriosis, or past gastrointestinal problems can be crucial in understanding your current symptoms.
Your medical history provides valuable context that can help healthcare professionals pinpoint the cause of your discomfort and recommend the most appropriate treatment.
Conclusion About Rectal Pain And Pressure
Rectal pain and pressure can stem from a variety of causes, each requiring specific attention. If you are experiencing these symptoms, visit Advanced Colorectal and General Surgery. Our expert colorectal specialist can help diagnose and treat the underlying cause so you can find relief.
Do not ignore any rectal pain or pressure, as early diagnosis can help prevent more serious complications from developing. Schedule a consultation with us today to receive personalised care and treatments.
Frequently Asked Questions About Rectal Pain And Pressure
Can Diet And Lifestyle Changes Alleviate Rectal Pain?
Yes, dietary and lifestyle modifications, such as increasing fibre intake, staying hydrated, and exercising regularly, can help alleviate rectal pain, particularly when related to constipation or haemorrhoids.
When Should I Seek Immediate Medical Attention For Rectal Pain?
Seek immediate medical attention for rectal pain if it’s accompanied by severe bleeding, intense abdominal pain, dizziness, fever, or sudden worsening of symptoms.
Are There Any Home Remedies For Mild Rectal Pain?
For mild rectal pain, warm sitz baths, over-the-counter pain relievers, and applying haemorrhoid creams can provide relief. However, keep in mind that they are not substitutes for professional medical advice.
Is Rectal Pain Common During Pregnancy?
Rectal pain is relatively common in pregnancy, often due to increased pelvic pressure and constipation, and should be discussed with a healthcare provider for appropriate management.