Think your symptoms are pointing to hernia? Learn the types of Hernia in Singapore and what you can do for treatment.
Continue readingWhat Does a Colorectal Surgeon Do?
Think you have a colorectal condition? A colorectal surgeon can help with treatment and surgery. Find out how.
Continue readingHow Gastroscopy Singapore helps diagnose digestive diseases?
Wonder how your digestive problem will be diagnosed? Learn why Gastroscopy Singapore is a reliable tool for diagnosing digestive conditions.
Continue readingPreparing For A Colonoscopy
Looking for preparation steps for a colonoscopy in Singapore? Learn what is needed for a successful colonoscopy screening at our clinic.
Continue readingEndoscopy: What to Expect
Undergoing a medical procedure for the first time can be a nerve-wracking experience, especially when you don’t know what to expect. Many patients in Singapore feel anxious about endoscopy, a standard procedure used to examine the body’s internal structures.
Understanding what endoscopy entails, from preparation to post-procedure care, can help alleviate these concerns and ensure you feel more confident and prepared.
What Is An Endoscopy Specialist?
Endoscopies are performed by an endoscopist or endoscopy specialist in Singapore, a medical professional trained in gastroenterology, surgery, or other relevant fields. They use specialised instruments, such as an endoscope—a flexible tube with a light and camera attached—to view and operate on internal organs such as the lungs and stomach.
Endoscopy specialists in Singapore diagnose, monitor, and sometimes treat conditions such as gastrointestinal bleeding, lung infections and gastric cancer. Patients undergoing endoscopy often find additional insights through gastroscopy screening in Singapore, which offers a more focused examination of the upper digestive tract.
Preparing For Your Appointment
Before The Appointment
Preparation for an endoscopy begins days before the actual procedure. Your endoscopy specialist will provide instructions based on the type of endoscopy you’re having.
To prepare for an endoscopy, inform your specialist about your medical history, including any allergies and all medications or supplements you take. Certain medications may need to be adjusted or temporarily discontinued.
You may need to follow a special diet a few days before the procedure, typically avoiding solid foods and sticking to clear liquids 24 hours before the endoscopy. You’ll need to cleanse your bowel for some types of endoscopy, especially colonoscopy. Clearing the bowel may involve taking a prescribed laxative solution to clear the intestines.
On The Day Of The Appointment
On the day of your endoscopy, ensure you follow all instructions meticulously. Most endoscopic procedures require fasting, so refrain from eating or drinking for at least 6 hours before the procedure.
Arrange for someone to drive you to and from the appointment, as sedatives or anaesthesia will be administered, impairing your ability to drive. Wear loose-fitting clothing to the appointment, as you may need to change into a hospital gown for the procedure.
The Endoscopy Procedure
What Happens During An Endoscopy
When you arrive for your endoscopy in Singapore, you’ll be greeted by the medical team and given an overview of the procedure. Here’s what typically happens:
- Preparation: You’ll change into a gown and be connected to devices that monitor your vital signs.
- Sedation: You’ll receive a sedative or anaesthesia to help you relax or sleep during the procedure.
- Insertion of the endoscope: The endoscope is gently inserted into your body through a natural opening, such as your mouth or rectum, depending on the type of endoscopy.
- Examination: The specialist uses the endoscope’s camera to examine the internal structures. Small instruments can be pushed through the endoscope to take tissue samples or perform minor treatments if necessary.
- Duration: The procedure usually takes 15 minutes to an hour, depending on its complexity.
Safety And Hygiene
Safety and hygiene are paramount in endoscopic procedures. The endoscope and all instruments are thoroughly sterilised to prevent infections. Doctors follow strict protocols to ensure a sterile environment and minimise any risk of complications.
Post-Procedure Care
Immediately After The Procedure
After the endoscopy, you’ll be taken to a recovery area, where the staff will observe you until the sedation wears off. Here’s what to expect:
- Observation: You’ll be observed for adverse reactions to the sedative or the procedure.
- Rest: It’s normal to feel groggy or sleepy. Rest until you feel alert enough to go home.
- Instructions: You’ll receive post-procedure care instructions, including dietary guidelines and activity restrictions.
Follow-Up
Follow-up care is essential to ensure proper recovery and address any findings from the endoscopy. Your endoscopy specialist in Singapore will discuss the results with you, often on the same day, if no biopsies were taken. If tissue samples were collected, it may take a few days to get the results.
Contact your specialist if you experience severe pain, fever, vomiting, or any unusual symptoms after the procedure. Your endoscopy specialist may recommend additional tests, treatments, or lifestyle changes depending on the results. Patients interested in a complete digestive health check should consider both endoscopy and colonoscopy screening in Singapore, as these procedures collectively enhance the detection of early-stage gastrointestinal conditions.
Endoscopy Specialist In Singapore
Advanced Colorectal & General Surgery’s endoscopy specialists are trained and experienced in various endoscopic procedures in Singapore. If you’re considering a gastrointestinal check-up, you might want to understand the different endoscopic procedures to determine the most suitable option. We prioritise patient comfort and safety, ensuring each procedure is conducted with the utmost care.
Our team is dedicated to providing comprehensive pre- and post-procedure support, guiding you through every step to ensure a smooth and stress-free experience.
To learn more about endoscopy, get in touch with us.
Anal Fissures: Surgical and Non-Surgical Treatments
If you experience excruciating pain during or after bowel movements, you might be suffering from an anal fissure. This condition can impact your daily life, making each trip to the bathroom uncomfortable.
Fortunately, anal fissures can be treatedIn this article, we discuss both surgical and non-surgical treatments for anal fissures, helping you make informed decisions about your well-being.
What Are Anal Fissures
Anal fissures are small tears in the anus lining that make bowel movements uncomfortable and painful. The pain may also be accompanied by itching, bleeding, and a visible tear in the skin around the anus. These fissures can affect anyone but are particularly common in adults aged 15 to 40.
Anal fissures are caused by:
- Constipation: Hard, dry stools can cause tears as they pass through the anal canal.
- Diarrhoea: Frequent loose or watery stools can irritate and tear the anal lining.
- Childbirth: Women may develop fissures due to the strain of delivery.
- Anal Intercourse: This can cause trauma to the anal lining.
- Underlying Conditions: Conditions like Crohn’s disease can cause chronic inflammation of the intestines, leading to fissures.
Non-Surgical Treatment Options
Most anal fissures can be managed with non-surgical treatments, especially if addressed early. Here are some effective non-surgical options.
Dietary Changes
Changing your diet is one of the simplest ways to treat and prevent anal fissures. Key dietary changes you can implement include:
- High-Fibre Foods: Incorporate fruits, vegetables, whole grains, and legumes for softer stools and make them easier to pass.
- Hydration: Drinking plenty of water helps keep stools soft.
- Avoiding Irritants: Limit intake of spicy foods, caffeine, and alcohol, which can irritate the digestive tract.
Medications
You can manage symptoms and promote healing of anal fissures with medication. These include:
- Stool Softeners: Over-the-counter stool softeners can ease bowel movements.
- Topical Anaesthetics: Creams or ointments containing lidocaine can reduce pain.
- Nitrate Ointments: These help relax the anal sphincter and enhance blood circulation to the area, promoting healing.
- Calcium Channel Blockers: Applied topically, these medications relax the anal sphincter muscles.
Sitz Baths
A sitz bath means sitting in warm water for 10-20 minutes several times daily, particularly after bowel movements. The warmth can soothe pain and itching, while increased blood flow to the area aids in healing. Regular sitz baths will also help maintain hygiene and prevent infection.
Lifestyle Modification
Changing your lifestyle can also support the healing process and prevent recurrence. Consider the following:
- Regular Exercise: Being physically active can help prevent constipation and promote digestive health.
- Proper Bowel Habits: Avoid straining during bowel movements, and go to the bathroom when you feel the urge.
- Good Hygiene: Gently clean the anal area with water, and pat dry after bowel movements.
Surgical Treatment Options
If non-surgical treatments fail to heal the anal fissure or if it becomes chronic, your doctor may recommend surgery. Understanding the preparatory steps for anal fissure surgery in Singapore is crucial for a successful outcome.
Lateral Internal Sphincterotomy
Lateral internal sphincterotomy is the most common surgical procedure for treating anal fissures. This surgery has a high success rate, relieving pain and promoting healing. A small cut is made in the internal anal sphincter muscle. The cut helps reduce the muscle tension, allowing the fissure to heal.
Non Surgical Alternatives
- Botox Injections: Botulinum toxin can be injected into the anal sphincter to paralyse the muscle, reducing spasms and pain temporarily.
Post-Surgery And Recovery
After surgery, proper care and adherence to recovery guidelines are essential:
- Pain Management: Pain is usually minimal after surgery but can be managed with prescribed medications.
- Wound Care: Clean the surgical site and keep it dry, and follow your surgeon’s instructions for wound care.
- Diet: Continue a high-fibre diet and stay hydrated to prevent constipation.
- Activity: Avoid straining yourself for a few weeks, but do light exercise as your doctor recommends.
- Follow-up: Attend all follow-up appointments to ensure proper healing.
How To Choose The Proper Treatment
Choosing the right treatment for anal fissures depends on the severity of the fissure, your overall health, and your response to initial treatments. If you’re trying to understand your symptoms, our explanation on anal fissures vs fistulas and their causes might help clarify your doubts.
It is best to speak to your healthcare provider about your symptoms and treatment options so you can discuss which treatment option is suitable for you. It’s essential to understand the recovery timeline if you opt for anal fissure surgery in Singapore. If distinguishing between an anal fissure and haemorrhoid seems challenging, our blog provides a clear explanation of the four main differences.
Consult A Colorectal Specialist For Anal Fissure Treatment And Surgery In Singapore
For personalised care and expert advice on treating anal fissures, consult the specialists at Advanced Colorectal & General Surgery. Our team of experienced colorectal surgeons in Singapore provides complete care, from diagnosis to treatment and recovery. We offer non-surgical and surgical options tailored to your needs, ensuring the best possible outcomes.
Colon cancer and treatments in Singapore
Colon cancer, a malignancy of the large intestine, is a significant health concern in Singapore. Given its increasing prevalence and the complexities involved in its treatment, it’s crucial to understand the disease, its progression stages, and the various treatment options available.
In Singapore, continuous improvements in colon cancer treatment protocols reflect the country’s commitment to medical excellence and patient care. This article provides an in-depth look at colon cancer, focusing on the stages of the disease, factors influencing treatment decisions and the support necessary for patients.
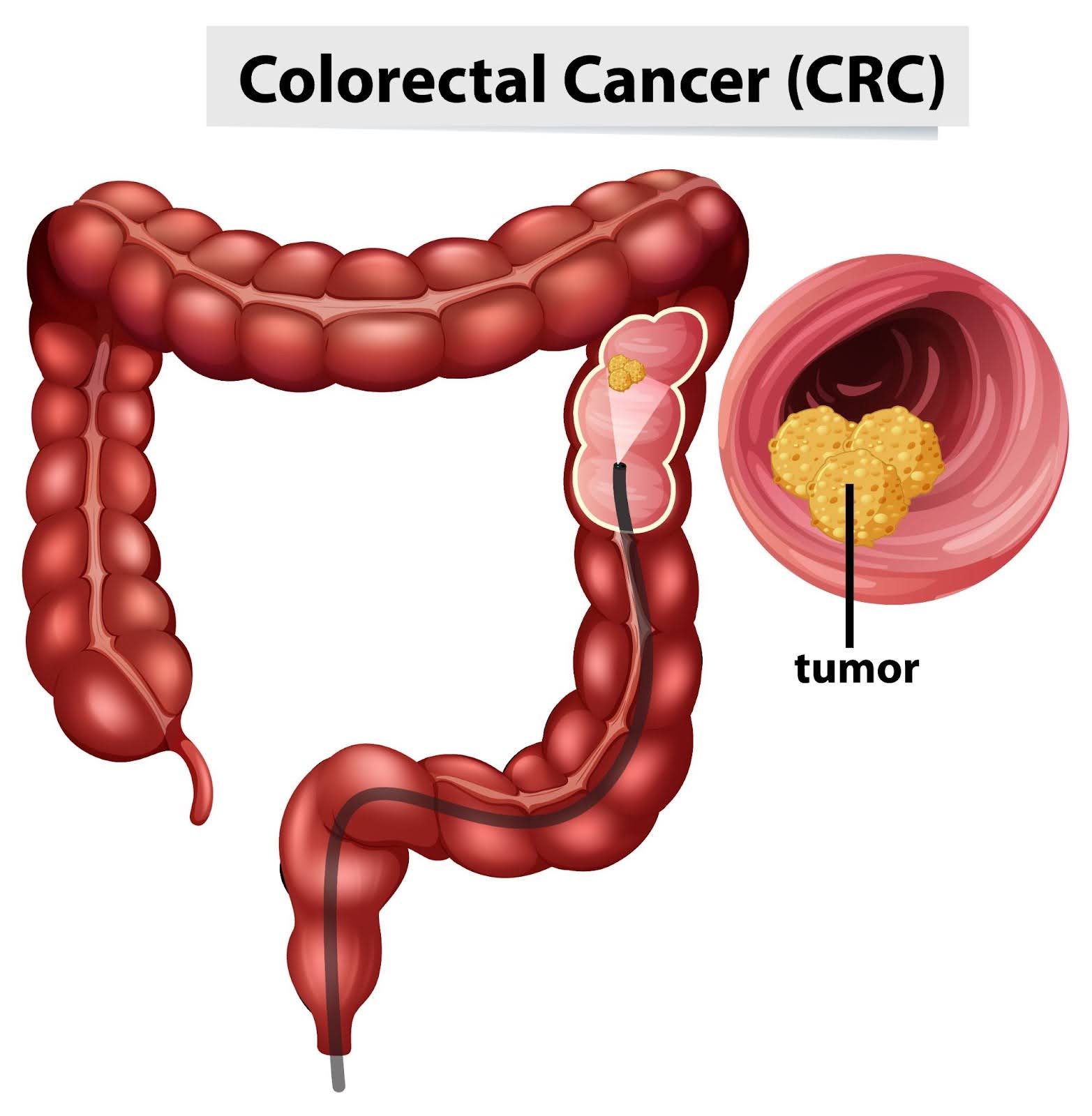
What Is Colon Cancer?
Colon cancer originates in the large intestine (colon), which is the final part of the digestive tract. It typically starts as small, noncancerous clumps of cells called polyps that form on the inside of the colon. Over time, some of these polyps can become colon cancers. Emphasising early detection, Singapore colorectal cancer screening programs are designed to identify precancerous conditions before they develop into full-blown cancer.
While the exact cause of colon cancer is not entirely understood, several risk factors have been identified, including age, a family history of the disease, certain genetic mutations, a diet high in red and processed meats, and lifestyle factors such as smoking and physical inactivity. With ongoing research and clinical trials, colorectal cancer treatment in Singapore continues to evolve, offering new hopes for better outcomes.
The Stages Of Colon Cancer
Colon cancer is classified into stages based on the extent of its spread. Understanding these stages is critical for determining the appropriate treatment strategy. Recognizing the signs can be crucial for catching potential issues early, enabling timely medical intervention and increasing the chances of a favourable outcome.
Stage 0 – Carcinoma In Situ
Stage 0, also known as carcinoma in situ, is the earliest form of colon cancer. At this stage, the cancerous cells are confined to the innermost layer of the colon’s lining and have not invaded deeper tissues or spread to other parts of the body. This stage is typically highly treatable, often through surgery to remove the localised area of abnormal cells.
Stage 1 – Early Stage Colon Cancer
In Stage 1, cancer has spread beyond the inner lining of the colon to the second and third layers of the colon wall, but it has not yet spread to the lymph nodes or distant sites. Treatment at this stage usually involves surgical resection of the affected section of the colon, often followed by a comprehensive monitoring plan to ensure that the cancer does not return.
Stage 2 – High-Risk Early Stage
Stage 2 colon cancer is more advanced, as the cancer has penetrated through the colon wall and may have reached nearby tissues but has not spread to the lymph nodes. It is further divided into sub-stages:
-
- Stage IIA: Cancer has spread through the muscle layer to the outermost layers of the colon or rectum.
-
- Stage IIB: Cancer has grown through the outermost layer but hasn’t reached nearby organs.
-
- Stage IIC: Cancer has grown through the outermost layer and into nearby structures.
Treatment for Stage 2 typically involves surgery to remove the tumour, possibly followed by chemotherapy, especially if there are high-risk features such as poorly differentiated cells or lymphovascular invasion.
Stage 3 – Regional Spread
At Stage 3, cancer has spread to nearby lymph nodes but not to other parts of the body. This stage is divided into three subcategories based on the number of affected lymph nodes and the extent of tumour invasion:
-
- Stage IIIA: Cancer has spread to up to three nearby lymph nodes and has penetrated the muscle layer.
-
- Stage IIIB: Cancer has spread to up to four to six nearby lymph nodes or into surrounding tissues.
-
- Stage IIIC: Cancer has spread to seven or more nearby lymph nodes but not to distant organs.
Treatment usually involves a combination of surgery, chemotherapy, and sometimes radiation therapy to address the cancer’s spread to lymph nodes.
Stage 4 – Metastatic Colon Cancer
Stage 4, or metastatic colon cancer, is the most advanced stage. Cancer has spread to distant organs such as the liver, lungs, or distant lymph nodes. This stage is further classified based on the extent and number of distant metastases:
-
- Stage IVA: Cancer has spread to one distant organ.
-
- Stage IVB: Cancer has spread to more than one distant organ or area.
-
- Stage IVC: Cancer has spread to the peritoneum (the lining of the abdominal cavity).
Treatment for Stage 4 focuses on controlling the cancer and relieving symptoms. This may include a combination of surgery, chemotherapy, targeted therapy, and immunotherapy to extend life and improve quality of life.
Colorectal cancer screening in Singapore is regarded as a key preventive measure that is highly encouraged among adults over the age of 50.
Factors Influencing Treatment Decisions
While we have covered various treatments above based on the stages of cancer, there are other factors in play, too:
-
- Patient’s overall health: Comorbidities and overall fitness can affect the choice of treatment.
-
- Genetic mutations: Specific genetic profiles, such as those involving KRAS, NRAS, and BRAF mutations, can influence treatment options, particularly concerning targeted therapies.
-
- Patient preferences: The patient’s quality of life, personal preferences, and treatment goals are essential in shaping the treatment plan.
Treatments
The treatment for colon cancer, as seen above, includes a variety of options. They may also be used in combination depending on the stage and characteristics of the cancer. Here are more details for each treatment:
-
- Surgery: The primary treatment for early-stage colon cancer, involves the removal of the tumour and surrounding healthy tissue. Types of surgery include polypectomy, colectomy, and proctectomy.
-
- Chemotherapy: Uses drugs to destroy cancer cells or stop them from growing. It is commonly used post-surgery in stages 2 and 3 and as a primary treatment for advanced stages.
-
- Radiation therapy: Employs high-energy radiation to kill cancer cells or shrink tumours. Though it is used for colon cancer, it is more commonly used for rectal cancer.
-
- Targeted therapy: Uses drugs or other substances to target specific molecules involved in cancer growth and spread. Commonly used drugs include cetuximab and bevacizumab.
-
- Immunotherapy: Boosts the body’s natural defences to fight cancer. It is an option for certain advanced cancers that have specific genetic mutations or markers.
-
- Palliative care: Focuses on relieving symptoms and improving the quality of life for patients with advanced cancer.
Supporting Patients Through Treatment
Supporting colon cancer patients involves a multidisciplinary approach that includes medical treatment, emotional support, and practical assistance.
-
- Multidisciplinary care teams: These teams consist of oncologists, surgeons, radiologists, nurses, and social workers who collaborate to provide comprehensive care.
-
- Patient education: Providing patients with detailed information about their diagnosis, treatment options, and side effects to empower them to make informed decisions.
-
- Psychosocial support: Offering counselling services and support groups to help patients and their families cope with the emotional impact of cancer.
-
- Financial assistance: Helping patients navigate financial resources and insurance options to ease the burden of treatment costs.
-
- Rehabilitation services: Providing physical therapy and nutritional counselling to help patients recover and maintain their health during and after treatment.
Colon Cancer Treatment In Singapore
Colon cancer can be daunting, but with expert care, it’s manageable and treatable. At Advanced Colorectal and General Surgery, we specialise in the comprehensive screening and treatment of colorectal cancer in Singapore. We are committed to providing personalised and compassionate support every step of the way.
Ongoing public education efforts emphasise the importance of regular colon cancer screening in Singapore as a critical step towards maintaining long-term health. The colorectal cancer treatment services in Singapore are not only advanced but also emphasise compassionate care, recognizing the emotional and physical challenges faced by patients.If you or a loved one is facing a colon cancer diagnosis or you want to learn more about our services, don’t wait. Contact us today to schedule a consultation.
Proctologist Vs Colorectal Surgeon: Is There A Difference?
Proctologists and colorectal surgeons are specialists a general doctor may recommend to patients experiencing symptoms or issues related to the lower digestive tract. This could be in the form of persistent rectal pain, bleeding, and irregular bowel movements.
What’s the difference between these two professions? None. They can be used interchangeably, although colorectal surgeons are preferred by doctors today who specialise in colon and rectum.
This article discusses these roles, detailing the evolution from proctologist to colorectal surgeon and explaining the conditions these specialists treat.
What Is A Proctologist?
The term proctologist originates from a time when the medical community began recognising the need for a speciality focused on diseases of the colon, rectum, and anus.
Back in 1835, the field of proctology was emerging in response to a gap in medical care. Many doctors were reluctant to treat these conditions, leading patients to seek help from less reputable sources, often resulting in mistreatment.
To address this, a group of doctors established the speciality of proctology, aiming to provide professional and effective care for these intimate and complex conditions.
Historically, a proctologist was a doctor who specialised in the rectum, anus, and sigmoid colon. Their focus was narrow, primarily dealing with diseases confined to the lower portion of the digestive system.
Common conditions treated by proctologists included haemorrhoids, anal fissures, fistulas, and chronic constipation issues.
The term “proctologist” emphasises a specialist’s expertise in diagnosing and treating disorders in the proctology area, using both medical and surgical methods.
When Did The Title Colorectal Surgeon Begin?
The transition from the term proctologist to colorectal surgeon was motivated by the need for clarity and precision in the scope of this medical speciality.
The term “proctologist” comes from the Greek word “proktos,” meaning anus, which inaccurately suggested that these specialists focused solely on the anal region. This narrow interpretation did not reflect the wide range of conditions treated by these doctors, including diseases of the colon, rectum, anus, and pelvic floor.
To better represent the comprehensive nature of their work, the designation evolved to “colon and rectal surgeon”, or colorectal surgeon in short, a term encompassing the full breadth of their expertise.
Colorectal surgeons in Singapore are professionals who have completed extensive education and training in both general surgery and specialised colorectal surgery.
They handle a wide variety of conditions, from benign diseases like haemorrhoids to more serious conditions such as colorectal cancer, using both surgical and non-surgical treatments.
Colorectal Surgeon Training And Qualifications
Becoming a colorectal surgeon in Singapore involves rigorous training and education. Initially, one must earn a medical degree over 5 to 6 years, followed by postgraduate medical training in various disciplines to secure general medical registration with the Singapore Medical Council.
Aspiring colorectal surgeons then undertake specialist general surgery training for around 5-6 years, gaining certification from professional bodies. Subsequently, they undergo advanced surgical training in colorectal surgery under expert supervision, including local and international opportunities.
To practise, they must pass exams and fulfil the Specialist Accreditation Board’s requirements, being registered as specialists in general surgery with a subspecialty in colorectal surgery.
Continuous professional development through Continuing Medical Education is essential to stay abreast of advancements. Singapore’s strict standards ensure its colorectal surgeons are highly qualified, often holding affiliations with prominent medical associations to enhance their expertise further.
Conditions Proctologists Or Colorectal Surgeons Treat And Manage

Colorectal surgeons are equipped with the expertise to diagnose, manage, and treat these conditions through a combination of medical treatments and surgical procedures. Their specialised training allows them to help patients suffering from these often complex and sensitive health issues.
- Haemorrhoids: Enlarged veins in the rectal region, leading to discomfort, itchiness, and bleeding.
- Anal Fissures: Minor lacerations in the anal skin, causing pain and bleeding with bowel movements.
- Anal Fistulas: Unusual pathways connecting the anal canal to the skin surrounding the anus, typically arising from infection.
- Anal Abscesses: Infections filled with pus located near the anus or rectum.
- Diverticulitis: Swelling or infection of tiny sacs (diverticula) in the colon walls.
- Colorectal Cancer: Tumours found within the colon or rectum, necessitating specialised surgical procedures.
- Crohn’s Disease: A variant of inflammatory bowel disease impacting any segment of the gastrointestinal tract, including the colon.
- Ulcerative Colitis: A chronic inflammatory bowel disease resulting in prolonged inflammation and ulcers within the colon and rectum.
- Pilonidal Disease: Persistent skin infection situated in the buttocks’ crease adjacent to the tailbone.
- Rectal Prolapse: The descent of the rectum, protruding through the anus.
- Faecal Incontinence: The inability to retain bowel contents leads to unintended stool leakage.
- Constipation: Persistent difficulty in stool passage, often needing clinical management.
- Rectocele: Protrusion of the rectum’s front wall into the vagina’s back wall.
- Colon Polyps: Lesions on the colon’s inner surface, potentially pre-cancerous.
- Pelvic Floor Dysfunction: Disorders affecting the pelvic floor muscles’ coordination and relaxation, necessary for bowel movements.
- Pruritus Ani: Persistent anal itching.
- Lynch Syndrome and Other Genetic Colon Cancer Syndromes: Genetic disorders elevate the risk for colon cancer and additional cancers.
Medical Procedures Colorectal Surgeons Perform

Colorectal surgeons perform a wide array of procedures to diagnose, manage, and treat various diseases, ranging from benign to life-threatening. People don’t know that they also do diagnostic evaluations or screenings apart from surgeries.
Colonoscopy
This is the most comprehensive screening tool for colorectal cancer. It is necessary to visually examine the entire colon and rectum. This allows the surgeon to check for any abnormal growths or polyps.
Colonoscopy is recommended as a routine screening tool starting at age 50, but earlier or more frequent screenings may be advised for those with a higher risk.
Flexible Sigmoidoscopy
The procedure also involves using a flexible tube to check the rectum and the lower part of the colon. While less invasive than a full colonoscopy, it does not allow the entire colon to be examined, so its use as a screening tool may be limited to specific circumstances.
CT Colonography (Virtual Colonoscopy)
This imaging procedure uses CT scans to create detailed images of the colon and rectum. It is recommended as a less invasive alternative to traditional colonoscopy for patients who are medically unable to undergo the latter.
Minimally Invasive Surgery
Minimally invasive surgery, including laparoscopic and robotic-assisted techniques, represents a significant advancement in colorectal surgery. These approaches involve making several small incisions through which specialised instruments and a camera are inserted to perform the surgery.
The benefits of minimally invasive surgery are manifold: reduced pain and scarring, shorter hospital stays, and faster recovery times compared to traditional open surgery.
Laparoscopic surgery is widely used for a variety of colorectal conditions, including the removal of cancerous growths, the repair of hernias, and the treatment of diverticulitis.
Major Resection Surgery
For advanced cases of colorectal cancer and other severe conditions, major resection surgery may be necessary. This surgery is done to remove the affected portion of the colon or rectum and possibly nearby lymph nodes.
Resection procedures are critical in the management of colorectal cancer, ensuring the complete excision of cancerous tissues while striving to preserve as much of the healthy bowel as possible.
Techniques vary depending on the location and extent of the disease, including total colectomy, partial colectomy, and low anterior resection.
Anorectal Surgery
Anorectal surgery addresses conditions affecting the anal region and lower rectum, such as haemorrhoids, anal fissures, and fistulas. These are common problems that can cause significant discomfort and impact the quality of life.
Hemorrhoidectomy, for instance, involves the removal of haemorrhoids, offering relief from bleeding, irritation, and swelling. Surgery for anal fissures typically aims to relax the anal sphincter muscle, reducing pain and facilitating healing.
For anal fistulas, various procedures can be performed to close the fistula tract and prevent recurrent infections. Anorectal surgery often benefits from minimally invasive techniques, reducing recovery time and improving patient comfort.
Conclusion About Proctologist Vs Colorectal Surgeon
Seek a colorectal surgeon when experiencing symptoms related to the colon, rectum, or anus or for routine screenings to prevent colorectal cancer.
Consider scheduling a visit to Advanced Colorectal and General Surgery. We offer same-day colonoscopy, allowing you to get a consultation and get fast results. Our resident colorectal specialist, Dr QM Leong, provides an honest diagnosis and compassionate care.
Frequently Asked Questions About Proctologist Vs Colorectal Surgeon
What Can I Expect During My First Visit To A Colorectal Surgeon?
During your first visit, the colorectal surgeon will review your medical history, perform a physical examination, and discuss your symptoms. Diagnostic tests, such as blood tests, colonoscopy, or imaging studies, may be recommended to understand your symptoms’ cause and create a suitable treatment plan.
Is Colorectal Surgery Safe?
Colorectal surgery is generally safe when performed by an experienced and qualified surgeon. As with any surgical procedure, there are risks involved, but advancements in surgical techniques, including minimally invasive surgery, have significantly reduced these risks and improved recovery times.
How Long Is The Recovery After Colorectal Surgery?
Recovery time varies depending on the type of surgery performed, the individual’s overall health, and the presence of any complications. Minimally invasive surgeries tend to have shorter recovery times, often allowing patients to return to normal activities within a few weeks. Your surgeon will provide specific guidance based on your situation.
How Do I Prepare For A Colonoscopy Or Other Diagnostic Procedures?
Preparation for a colonoscopy typically involves following a special diet the day before the procedure and taking a laxative to empty the colon. Your colorectal surgeon will provide detailed instructions on how to prepare, including dietary restrictions and any necessary medication adjustments.
Feeling Rectal Pain And Pressure? Here Are 11 Possible Causes
Rectal pain and pressure can be uncomfortable and sometimes alarming symptoms. These sensations can stem from a variety of causes, ranging from mild and manageable conditions to more severe health issues.
This article explores the potential causes, their symptoms, and available treatments. It also tackles the diagnostic procedures to determine the exact cause of rectal pressure and pain and for effective pain relief.
1. Haemorrhoids
Haemorrhoids can cause discomfort, itching, pain, bleeding, and pain when sitting and during bowel movements. Haemorrhoids are swollen veins that may be located internally (inside the rectum) or externally (under the skin around the anus). External haemorrhoids might produce more pain and swelling in the area of the anus.
Haemorrhoids Treatments
Treatment for haemorrhoids often includes over-the-counter creams or suppositories, warm baths, and keeping the anal area clean. Dietary changes, like increasing fibre intake, can help prevent constipation and straining, which can exacerbate haemorrhoids.
In severe cases, procedures like rubber band ligation, sclerotherapy, or surgery may be recommended.
2. Anal Fissures
An anal fissure is a small tear in the thin, moist tissue lining the anus. Fissures can cause pain, especially during bowel movements, and bleeding. The pain is often described as sharp and severe. People may also experience spasms in the ring of muscle at the end of the anus (anal sphincter).
Anal Fissure Treatments
Most anal fissures heal with home treatments, such as warm baths, increased fibre intake, and over-the-counter pain relievers.
Applying topical anaesthetics to numb the area can help relieve pain during bowel movements. In cases where fissures do not heal with home treatment, prescription creams or surgery may be required.
3. Proctitis
Proctitis is inflammation of the lining of the rectum. It can cause symptoms such as a frequent or continuous feeling of needing to have a bowel movement, rectal bleeding, mucus in the stool, rectal pain, and pain on the left side of the abdomen.
People with proctitis might also experience a sensation of fullness in the rectum.
Proctitis Treatments
Treatment of proctitis depends on the cause. If an infection causes it, antibiotics or antiviral medications may be prescribed. For inflammatory causes, such as inflammatory bowel disease, medications to reduce inflammation might be used. Dietary changes and symptom management, like sitz baths, can also help.
4. Constipation

Constipation or difficulty passing hard or lumpy stools can cause rectal pain. Due to the straining during bowel movements, a sensation of incomplete evacuation, and discomfort or pain in the abdomen and rectum.
Constipation Treatments
Treatment often includes lifestyle changes like increasing fibre intake, drinking more fluids, and regular exercise. You can take over-the-counter laxatives for short-term relief. For chronic constipation, a healthcare provider might recommend prescription medications or, in rare cases, surgery.
5. Abscesses
An anal or rectal abscess, which is a painful collection of pus, may cause severe pain, swelling, redness, and tenderness in the area around the anus or rectum. Other symptoms can include fever, fatigue, and a noticeable lump or mass at the anal opening. The pain usually intensifies during bowel movements.
Abscess Treatments
Treatment usually involves surgical drainage of the abscess, which is often done under local anaesthesia. Antibiotics may be prescribed if an infection is present. Pain management and keeping the area clean are important aspects of post-procedure care.
6. Inflammatory Bowel Disease (IBD)
Crohn’s disease and ulcerative colitis cause chronic inflammation of the digestive tract and can lead to rectal pressure or pain.
Among the other common symptoms of these Inflammatory Bowel Diseases include diarrhoea, abdominal pain, blood in the stool, weight loss, and fatigue. The severity of symptoms can vary and often fluctuates with periods of remission and flare-ups.
IBD Treatments
The goal of the treatment for IBD is to reduce inflammation and suppress the immune system. Doctors may recommend corticosteroids, immunomodulators, and biologics.
Dietary changes and nutritional support may also be necessary. In severe cases, surgery to remove a damaged portion of the digestive tract might be required.
7. Rectal Prolapse
Rectal prolapse involves the rectum stretching and protruding from the anus. It can cause symptoms like a feeling of a bulge or lump in the anus, discomfort or pain during bowel movements, mucus or blood discharge from the protruding tissue, and incontinence (difficulty controlling bowel movements).
Rectal Prolapse Treatments
The treatment for rectal prolapse may include lifestyle changes, pelvic floor exercises, or stool softeners to reduce straining. In more severe cases, surgery may be necessary to repair the prolapse.
Several surgical options are available, and the choice depends on the patient’s overall health, age, and the severity of the prolapse.
8. Colorectal Cancer
Colorectal cancer patients often experience changes in bowel habits (like diarrhoea or constipation), rectal bleeding or blood in the stool, persistent abdominal discomfort (like cramps, gas, or pain), a feeling that the bowel doesn’t empty completely, weakness or fatigue, and unexplained weight loss.
In the early stages, colorectal cancer might not cause any symptoms.
Colon Cancer Treatments
Depending on the stage of colon cancer, treatments may include surgery (to remove cancer), radiation therapy, chemotherapy and targeted drug therapy. Early detection significantly improves the prognosis.
9. Sciatica

Sciatica can cause rectal pain and pressure. While sciatica pain is usually felt in the lower back and legs, it can sometimes affect the pelvic area and cause discomfort in regions such as the rectum. This is because the nerve pain or nerve compression causing sciatica can sometimes extend to these areas.
However, rectal pressure is not the most common symptom of sciatica. Most people with this condition experience lower back pain, hip pain, and burning or tingling down the leg. It usually affects only one side of the body.
Sciatica Treatments
Treatment options include physical therapy, and medications (like pain relievers, anti-inflammatories, and muscle relaxants), and, in severe cases, surgery. Home remedies like heat/ice therapy and exercises can also provide relief.
10. Endometriosis
This condition happens when a person’s uterine lining grows outside the uterus. Endometriosis can cause rectal pain in women if it involves the bowel or is located near the rectum.
More common symptoms include painful periods, pain during intercourse, urinating, and bowel movements. It can also accompany excessive bleeding and infertility.
Endometriosis Treatments
Treatment includes pain medications, hormone therapy (like contraceptives or other hormonal treatments), and surgery (to remove endometrial tissue). The choice of treatment depends on the severity of symptoms and whether the woman wishes to become pregnant.
11. Fibroids
Uterine fibroids are benign tumours that develop in the uterus. Large fibroids can cause rectal pain by putting pressure on the rectum.
However, the primary symptoms are heavy menstrual bleeding, prolonged periods, pelvic pressure or pain, frequent urination, difficulty emptying the bladder, constipation, and backache or leg pains.
Fibroid Treatments
Treatment options include medications (to regulate menstrual cycle or shrink fibroids), noninvasive procedures (like MRI-guided focused ultrasound surgery), minimally invasive procedures (like uterine artery embolisation), and traditional surgical procedures (like myomectomy or hysterectomy).
Diagnosing The Cause Of Rectal Pressure And Pain

Determining the exact cause of rectal pain and pressure can be challenging, as several different conditions can produce similar symptoms. However, certain steps and considerations can help narrow down the potential causes.
Note The Specific Symptoms And Their Patterns
Keep track of your symptoms, including the nature of the pain (sharp, dull, throbbing), its duration, any triggers, and associated symptoms like bleeding, changes in bowel habits, or weight loss. Symptoms can often provide clues about the underlying condition.
Consult A Healthcare Professional
This is the most important step. A healthcare provider, such as a colorectal specialist, can conduct a thorough examination and ask detailed questions about your medical history and symptoms.
Based on the initial evaluation, your doctor may recommend tests such as:
- Digital Rectal Exam (DRE): The doctor examines the rectum manually to check for abnormalities.
- Anoscopy or Proctoscopy: Instruments are used to visualise the inside of the rectum.
- Colonoscopy Screening: For a more extensive examination of the entire colon and rectum, the doctor may recommend a colonoscopy.
- Imaging Tests: Ultrasound, MRI, or CT scans can provide detailed images of the rectum and surrounding areas.
- Stool Tests: This is conducted to check for blood or signs of infection in the stool sample.
- Blood Tests: This is necessary to look for signs of infection, inflammation, or other markers that might indicate a specific condition.
Consider Your Medical History
Pre-existing conditions such as inflammatory bowel disease, endometriosis, or past gastrointestinal problems can be crucial in understanding your current symptoms.
Your medical history provides valuable context that can help healthcare professionals pinpoint the cause of your discomfort and recommend the most appropriate treatment.
Conclusion About Rectal Pain And Pressure
Rectal pain and pressure can stem from a variety of causes, each requiring specific attention. If you are experiencing these symptoms, visit Advanced Colorectal and General Surgery. Our expert colorectal specialist can help diagnose and treat the underlying cause so you can find relief.
Do not ignore any rectal pain or pressure, as early diagnosis can help prevent more serious complications from developing. Schedule a consultation with us today to receive personalised care and treatments.
Frequently Asked Questions About Rectal Pain And Pressure
Can Diet And Lifestyle Changes Alleviate Rectal Pain?
Yes, dietary and lifestyle modifications, such as increasing fibre intake, staying hydrated, and exercising regularly, can help alleviate rectal pain, particularly when related to constipation or haemorrhoids.
When Should I Seek Immediate Medical Attention For Rectal Pain?
Seek immediate medical attention for rectal pain if it’s accompanied by severe bleeding, intense abdominal pain, dizziness, fever, or sudden worsening of symptoms.
Are There Any Home Remedies For Mild Rectal Pain?
For mild rectal pain, warm sitz baths, over-the-counter pain relievers, and applying haemorrhoid creams can provide relief. However, keep in mind that they are not substitutes for professional medical advice.
Is Rectal Pain Common During Pregnancy?
Rectal pain is relatively common in pregnancy, often due to increased pelvic pressure and constipation, and should be discussed with a healthcare provider for appropriate management.
How Fast Do Colon Polyps Grow And Become Colon Cancer?
Colorectal cancers start as polyps. Over time, the cells in these polyps can undergo genetic changes, causing the cells to multiply uncontrollably, leading to cancer.
How quickly do colon polyps grow before they become cancerous? The growth rate varies significantly depending on the type of polyp and individual factors. Generally, they grow slowly over several years.
This article further explores the factors influencing how fast polyps grow in the colon, the factors influencing their growth, and ways to prevent colorectal cancer.
It Takes 10 Years For Colon Polyps To Grow
It can take about 10 years for a small colon polyp to develop into colorectal cancer, although this timeline can vary. According to a study, colonic polyps can invade the colonic wall and degenerate into cancer between 5 to 15 years.
The growth rate can be affected by the type of polyp, genetics, diet, lifestyle, and the presence of conditions like familial adenomatous polyposis (FAP) or Lynch syndrome, which can lead to a faster development of polyps and a higher risk of colon cancer.
So, even though it can take a decade for polyps to grow, this doesn’t mean you should wait or forget about getting checked for colorectal cancer. It’s a big reason why you should get a colonoscopy regularly.
Types Of Colon Polyps
A colonoscopy is a key screening tool used to identify and remove colon polyps. The doctor will classify the colon polyps found in the large intestine into two types: adenomatous and hyperplastic.
Adenomatous Polyps (Adenomas)
These are considered pre-cancerous and are the type most associated with developing colon cancer. They can take many years to develop into cancer, typically 10 to 15 years. Adenomatous polyps, particularly those larger than 1 cm or with more villous features, are more likely to become cancerous.
Hyperplastic Polyps and Inflammatory Polyps
These are generally not considered pre-cancerous. They are more common and usually don’t carry the same risk of developing cancer as adenomas do. Their growth rate is similar to that of adenomas, but they are less likely to develop cancer.
Other Factors That Can Influence The Polyps Growth Rate

In addition to the type of colon polyps, many other factors can affect their growth and their potential to become cancerous.
-
- Size of Polyp: Polyps larger than 1 cm have a significantly increased risk of containing cancerous cells. According to the American Cancer Society, the likelihood of a larger polyp being cancerous is higher than that of a smaller polyp.
-
- Number of Polyps: Individuals with multiple polyps, a condition known as polyposis, have a higher risk for colorectal cancer. Research indicates that the number of polyps correlates with the risk of colorectal cancer.
-
- Genetic Factors: Conditions like familial adenomatous polyposis (FAP) and Lynch syndrome are associated with a higher risk and more rapid growth of polyps. FAP, for example, leads to hundreds to thousands of polyps at a young age and nearly a 100% risk of colorectal cancer if not managed.
-
- Age: Polyp prevalence increases with age. Studies have shown that the incidence of adenomas increases significantly in individuals over 50 years of age, which is why colon cancer screening recommendations often start at this age.
-
- Diet and Lifestyle: Diets high in red and processed meats and low in fibre, fruits, and vegetables are linked with an increased risk of colorectal cancer. Obesity, smoking, and physical inactivity are also risk factors. A study in the “Journal of Nutrition” highlighted the role of diet in polyp development.
-
- Ethnicity and Race: African Americans are at a higher risk for colorectal cancer and may develop polyps at a younger age. This disparity suggests a potential difference in polyp growth rates among different ethnic groups, as noted in the American Journal of Gastroenterology research.
-
- Inflammatory Bowel Disease: Chronic inflammation from conditions like ulcerative colitis or Crohn’s disease is associated with Dysplasia and an increased risk of colorectal cancer. Studies in the “Gastroenterology” journal have shown that the risk of cancer increases the longer a person has inflammatory bowel disease.
-
- Previous Polyp History: A history of adenomas, especially advanced adenomas, is a decisive risk factor for the development of subsequent adenomas or colorectal cancer. The risk increases with the number and size of previously removed polyps, as indicated in studies.
-
- Family History: A family history of polyps or colorectal cancer increases the risk. Studies suggest that first-degree relatives of patients with colon cancer or adenomatous polyps have a two to three times higher risk of developing colorectal cancer or polyps themselves.
Screening And Diagnostic Procedures For Colon Polyps
Most polyps do not turn into cancer. However, removing them and analysing them is a key step in preventing colorectal cancer. Regular colorectal cancer screening, especially for individuals at higher risk (due to age, family history, genetic factors, etc.), is crucial for early detection and effective management.
Doctors use a combination of screening methods and diagnostic procedures to determine if colon polyps are cancerous. The process typically involves the following steps:
-
- Colonoscopy: This is the most common and effective method for detecting colon polyps using a colonoscope. If polyps are found in the colon, they can often be removed during the procedure.
-
- Polyp Removal: Polyps found during a colonoscopy are usually removed using tools passed through the colonoscope. This is important not only for diagnosis but also for prevention, as removing polyps can prevent them from turning into cancer.
-
- Histopathological Examination: The removed polyps are then sent to a laboratory for histopathological examination to identify their type and check for cancer signs.
-
- Assessing Dysplasia: The pathologist looks for Dysplasia. As mentioned, Dysplasia is a pre-cancerous condition, and its presence in a polyp is a strong indicator of potential for developing into cancer.
-
- Genetic Testing of the Polyp: Sometimes, genetic testing is performed on the polyp tissue to identify specific genetic mutations. This can help in assessing the risk of colorectal cancer and in guiding treatment decisions, particularly in hereditary cancer syndromes.
- Follow-Up Surveillance: Doctors will recommend a follow-up schedule for future colorectal screenings after polyps are removed and analysed. The frequency of follow-up colonoscopies depends on the number, size, and type of polyps and whether they contain cancer cells.
What Happens If Colon Polyps Are Cancerous
If colon polyps are found to be cancerous, the course of action and treatment will depend on various factors, including the cancer stage, the polyp’s size and location, and the patient’s overall health. Here’s a general outline of what might happen:
-
- Staging the Cancer: The next step is determining the cancer stage if a polyp is found to be cancerous. This involves assessing how deeply the cancer has penetrated the colon or rectum wall and whether it has spread to other parts of the body. Staging may involve additional tests like CT scans, MRIs, or ultrasounds.
-
- Surgical Intervention: Surgery is a standard treatment for colorectal cancer. Removing the polyp during the colonoscopy might be sufficient if the cancer is in its early stages and confined to the polyp. For larger cancers, more extensive surgery may be needed to remove the part of the colon or rectum where the cancer is located.
-
- Additional Treatments: If the cancer is more advanced or if there’s a higher risk of it coming back, additional treatments might be necessary. Depending on the colon cancer stage, the treatment can include chemotherapy, radiation therapy, or targeted therapy.
- Follow-up Care: After treatment, patients are required to do regular visits to the doctor and possibly additional colonoscopies or other tests to monitor for any signs of cancer returning or new polyps forming.
Ways To Prevent Colon Polyps From Becoming Colon Cancer

Aside from regular colon cancer screening, there are lifestyle changes that you can incorporate to stop colon polyps from growing or forming at all.
-
- Adopt a healthy diet: Eat more fruits, vegetables, whole grains, and legumes to boost fibre. Reduce red or processed meat like bacon and sausages as they are linked to an increased risk of colorectal cancer. You should also consume foods rich in calcium and vitamin D.
-
- Maintain a Healthy Weight: Obesity increases the risk of colon cancer and polyps. Aim for a healthy weight through diet and exercise for at least 30 minutes on most days of the week.
-
- Avoid Tobacco and Limit Alcohol: Smoking is a known risk factor for colorectal cancer and polyps. Quitting smoking can reduce this risk. You must also limit alcohol consumption.
-
- Consider Aspirin or Other Nonsteroidal Anti-inflammatory Drugs (NSAIDs): Some studies suggest that aspirin or other NSAIDs may help reduce the risk of polyps. However, these should only be taken under a doctor’s advice due to potential side effects.
Conclusion About How Fast Colon Polyps Grow
The growth rate of colon polyps can vary significantly, but generally, they develop over years rather than months. While not all polyps will turn into cancer, some can, especially if they’re left undetected and untreated. This slow growth rate highlights the importance of regular screenings so you can catch them earlier for better prognosis.
At Advanced Colorectal and General Surgery, we offer same-day colonoscopy. You will undergo consultation and screening all in the same day.
Our colorectal specialist will provide an in-depth diagnosis to help you understand your unique health needs and risks. Contact us to book a consultation today!
Frequently Asked Questions About How Fast Colon Polyps Grow
Do Colon Polyps Grow Back?
Yes, colon polyps can grow back, but it’s not inevitable. The likelihood of polyps reappearing depends on factors like the type of polyps initially removed, the number of polyps, and your genetic predisposition. People who have had polyps before are at a higher risk of developing new polyps in the future.
How Fast Do Colon Polyps Grow Back?
The growth rate of new polyps can vary. Typically, it takes several years for new polyps to develop and grow. The exact timeline can depend on individual factors like genetics, lifestyle, and certain medical conditions. Regular follow-up screenings, like colonoscopies, are recommended to monitor and manage this risk.
Do Colon Polyps Cause Constipation?
In most cases, small colon polyps do not cause symptoms and are usually not associated with constipation. However, larger polyps might cause bowel habit changes, including constipation. This is more common if the polyp partially obstructs the colon, though such large polyps are less common.
Is There Any Pain Associated With Colon Polyps?
Colon polyps themselves usually don’t cause pain. If a polyp grows large enough to cause obstruction or significant irritation in the colon, there might be discomfort or pain, but this is relatively rare.