Explore hernia repair treatment in Singapore with our comprehensive 2025 guide, covering minimally invasive options for a quick recovery.
Continue readingGastroscopy: What It Is, When You Need It and What to Expect
Having gastrointestinal issues? Looking for a clinic in Singapore for gastroscopy services? Here’s all you need to know to make an informed decision.
Continue readingChoosing a Gastroscopy Doctor in Singapore: What You Need to Know
Nervous about getting a gastroscopy? Discover how the right doctor and the right questions can make the experience less stressful.
Continue readingHernia Care in Singapore: Techniques and Treatments
Learn how hernias affect your health and explore modern, minimally invasive treatment options in Singapore. Find out why timely care makes all the difference.
Continue readingTips to Prepare and Recover from Colorectal Surgery in Singapore
Learn how to prepare for and recover from colorectal surgery in Singapore. Get expert tips on pre-surgery care, post-operative recovery and long-term health from Advanced Colorectal and General Surgery.
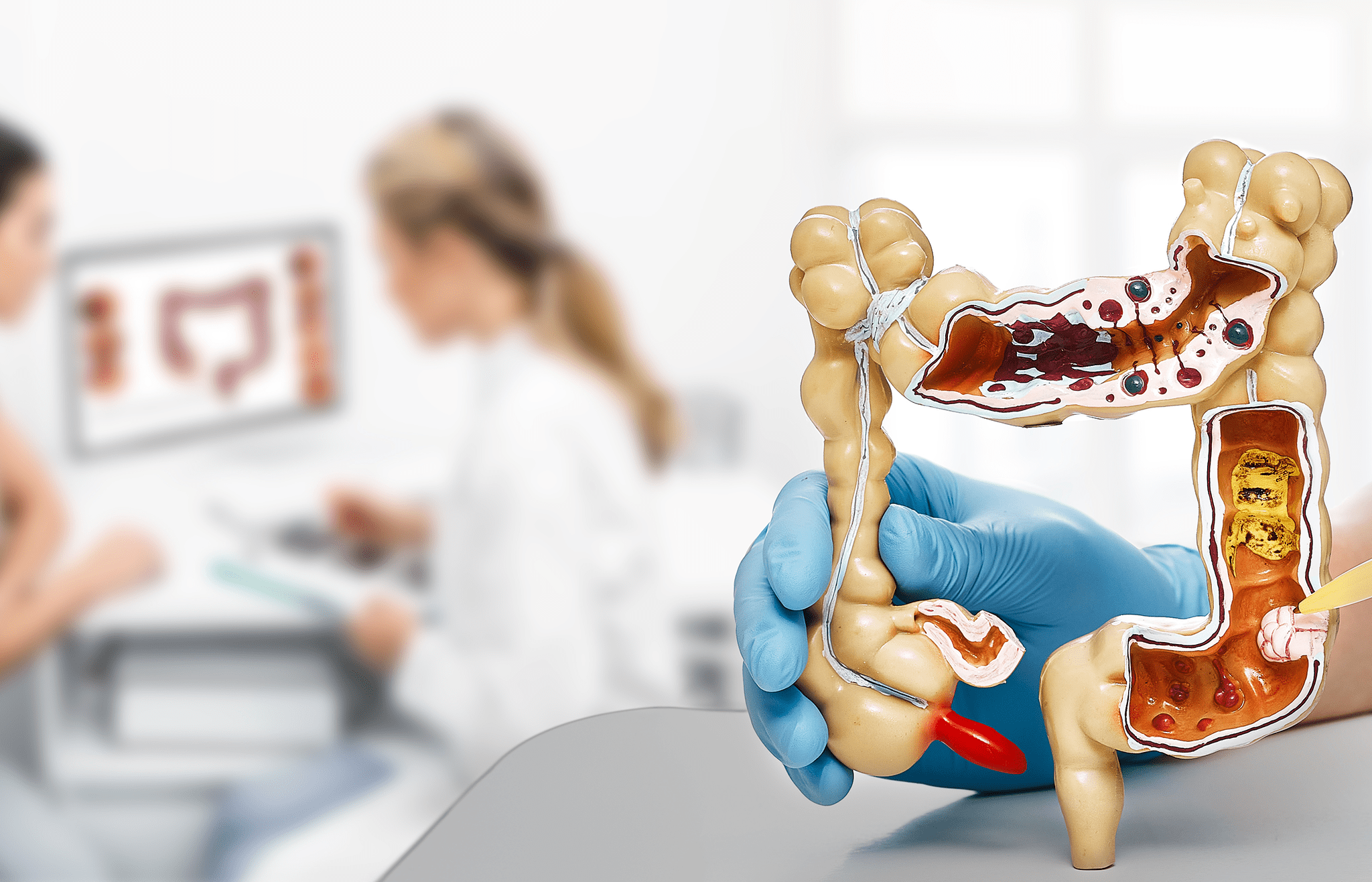
Continue readingA Guide to Colon Cancer Staging and Treatment Options
A doctor discusses colon cancer staging with a patient, using a detailed chart to explain the progression stages.
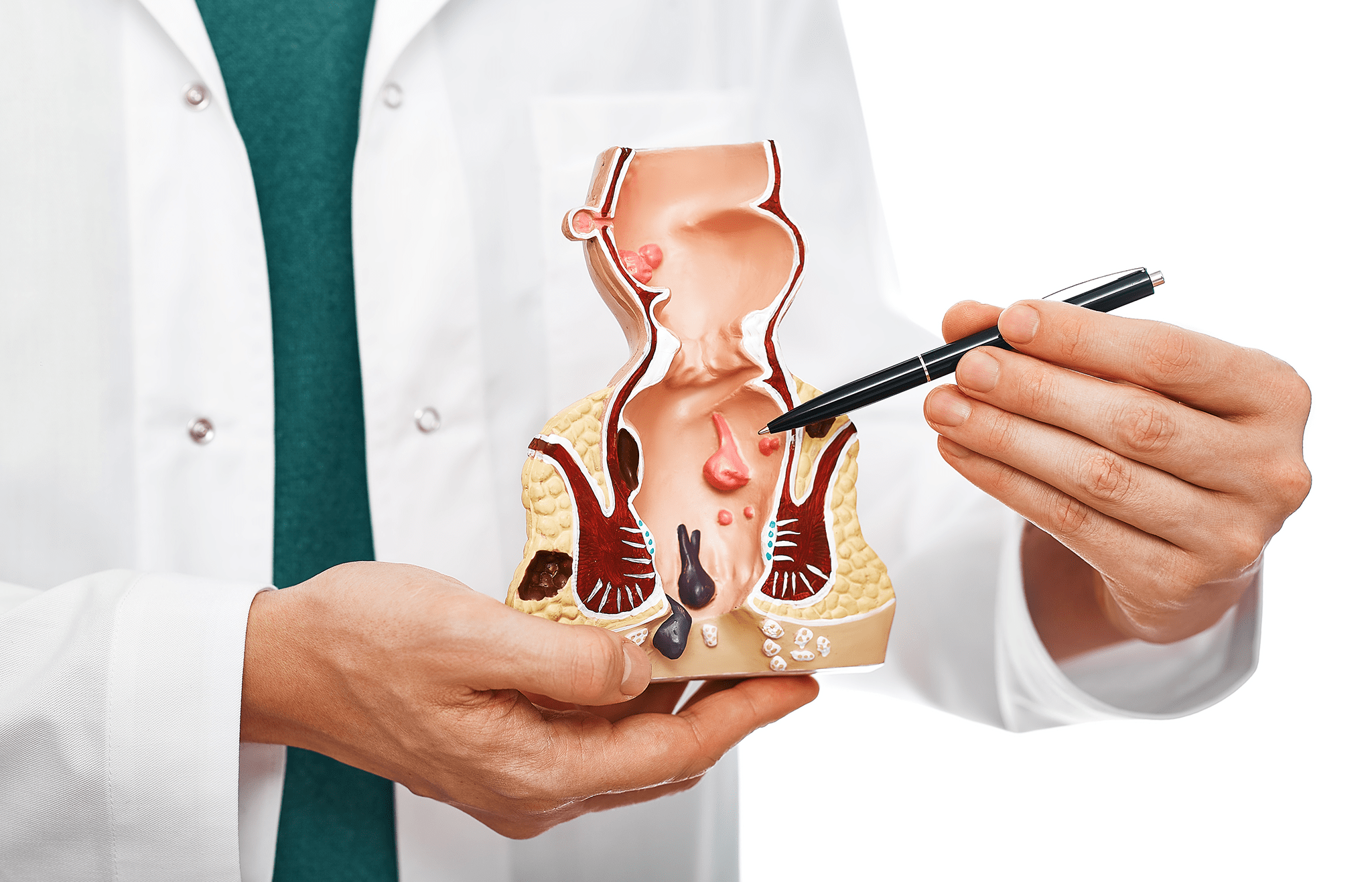
Continue readingNon-surgical vs Surgical Treatments for Piles: Which is Right for You?
Struggling with piles? Discover tailored treatments, from dietary changes to minimally invasive surgery, and find expert care at Advanced Colorectal and General Surgery in Singapore.
Continue readingAll You Need to Know About Colorectal Cancer Testing
Hernia: Symptoms & Treatment
Think your symptoms are pointing to hernia? Learn the types of Hernia in Singapore and what you can do for treatment.
Continue readingWhat Does a Colorectal Surgeon Do?
Think you have a colorectal condition? A colorectal surgeon can help with treatment and surgery. Find out how.
Continue reading