Diverticular Disease In Singapore | Symptoms, Complications, & Treatments
Insurance
Our surgery is on the panel of most of the major insurance companies and if you are covered by corporate insurance, you may be entitled to a cashless visit to our clinic.
Get In Touch
Table of Contents
Introduction
Diverticular disease in Singapore is a common health condition that affects the colon and may cause serious complications. It is characterised by pouches of inflamed tissue (diverticula) in the wall of the large intestine. It affects people primarily over 40 years old and it can be treated with surgery or medications. Only a small number of patients will require surgery for it.
To understand more about the diverticular disease in Singapore, Dr QM Leong has provided a comprehensive explanation of its causes and symptoms. He also explains the possible complications and treatment plans to manage this disease.
What Is Diverticular Disease, And What Causes It?
Diverticular disease is a prevalent gastrointestinal condition that affects a significant portion of the global population. Its prevalence varies by region, but it is more commonly observed in industrialised or developed countries like Singapore due to urbanisation and diet.
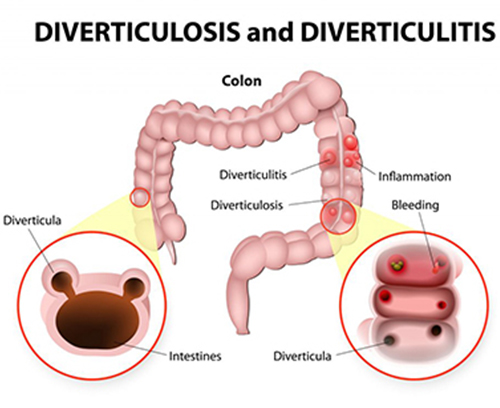
As mentioned, this condition is characterised by the presence of diverticula or small pouches forming in the walls of the colon (large intestine). These pouches can become inflamed or infected, leading to various health issues. There are two main forms of diverticular disease: diverticulosis and diverticulosis.
Diverticulosis: This is the presence of diverticula in the colon without inflammation or infection. Many people with diverticulosis may not experience any symptoms or even be aware of its presence.
Diverticulitis: This is a more serious condition where the diverticula becomes inflamed or infected. This can cause symptoms such as abdominal pain, fever, nausea, and changes in bowel habits.
The exact causes of diverticular disease are not fully understood, but several factors are believed to contribute to its development. Diverticular disease includes two main conditions: diverticulosis and diverticulitis. Here are some of the factors associated with these conditions:
- Ageing: One of the primary risk factors for diverticular disease is age. It becomes more common as people get older, and the risk increases with advancing age.
- Low-Fiber Diet: A low-fibre diet is considered a significant contributor to the development of diverticular disease. A diet that lacks sufficient dietary fibre can lead to constipation and hard stools, which can increase the pressure in the colon. This increased pressure may contribute to the formation of diverticula (small pouches) in the colon wall.
- Genetics: There may be a genetic component involved in the susceptibility to diverticular disease. It tends to run in families, suggesting that there may be a genetic predisposition to the condition.
- Lifestyle Factors: Certain lifestyle choices and conditions can increase the risk of diverticular disease, including:
- Smoking: Smoking has been associated with an increased risk of diverticular disease.
- Obesity: Being overweight or obese can raise the risk of developing diverticulosis and diverticulitis.
- Lack of Physical Activity: A sedentary lifestyle can contribute to constipation and may increase the risk of diverticular disease.
- Changes in Colonic Pressure: Elevated pressure in the colon, often associated with straining during bowel movements, can contribute to the formation of diverticula.
What Are The Common Symptoms Of Diverticular Disease In Singapore?
Diverticula are sac-like pouches that protrude from the smooth muscular layer of the colon with age. They tend to develop where the muscles are weakest, or at areas where penetrating vessels cross through the muscles.
They are caused by increased pressure along these weakened areas, such as during constipated bowel movement, being overweight and living a sedentary lifestyle, or due to a low-fibre diet.
The presence of diverticula, and consequently diverticular disease in Singapore, is more common in people over the age of 40 and affects up to 50% of people over the age of 60. Generally, diverticula exhibit no symptoms and require no treatment. Consequently, diverticula are usually only discovered during a colonoscopy or CT scan or when patients exhibit symptoms.
Both diverticular disease and diverticulitis exhibit similar symptoms, with diverticulitis having more intense and severe ones
Symptoms of Diverticulosis:
- Most Often Asymptomatic: Many people with diverticulosis do not experience any noticeable symptoms, and the condition is often discovered incidentally during medical tests or screenings.
- Mild Discomfort: Some individuals with diverticulosis may experience mild symptoms such as crampy abdominal discomfort, bloating, or irregular bowel habits, but these symptoms are generally not severe.
Symptoms of Diverticulitis (Inflamed or Infected Diverticula):
- Abdominal Pain: This is the most common symptom of diverticulitis. The pain is usually localized in the lower left side of the abdomen but can occur on the right side as well. It is often described as sharp or persistent and can be severe.
- Fever: Diverticulitis can lead to fever of 38C or higher and chills, especially if there is an infection.
- Changes in Bowel Habits: Individuals with diverticulitis may experience changes in their bowel habits, including diarrhoea or constipation.
- Nausea and Vomiting: Some people with diverticulitis may feel nauseous and may even vomit.
- Loss of Appetite: Diverticulitis can lead to a decreased appetite.
- Bloating and Gas: Abdominal bloating and excessive gas can occur in some cases.
- Rectal Bleeding: In more severe cases, diverticulitis can lead to rectal bleeding, which may present as bright red or maroon-coloured blood in the stool.
Complications Of Diverticulitis
The inflammation of the diverticula caused by diverticulitis can lead to other conditions beyond just fever and pain.
About 25% of people with acute diverticulitis develop complications, which may include:
- Abscess: In cases of severe diverticulitis, pus may collect within the inflamed diverticulum, leading to the formation of an abscess. This can cause localized pain and may require drainage or treatment.
- Stenosis: Prolonged inflammation and scarring can result in the narrowing of the bowel, known as stenosis. This can lead to bowel obstruction, causing symptoms such as abdominal cramping and changes in bowel movements.
- Fistula: Fistulas are abnormal connections that can form between different sections of the bowel or between the bowel and nearby organs, such as the bladder or vagina. These connections can lead to various symptoms, depending on their location.
- Peritonitis: Peritonitis is a severe and potentially life-threatening complication that can occur if an inflamed or infected diverticulum ruptures, spilling bowel contents into the abdominal cavity. Peritonitis requires immediate medical attention and surgical intervention.
If symptoms worsen or complications are suspected, prompt medical evaluation and intervention are crucial to prevent further harm and ensure appropriate treatment.
Treatments For Diverticular Disease In Singapore
As with other conditions, prompt and effective treatment for diverticulosis and diverticulitis is key to avoiding more severe health outcomes. Treatment depends on the severity of conditions, which may range from medicines and eating a healthier diet to undergoing major surgery to remove affected sections of one’s large intestine.
Diverticulosis Treatments
There are various treatments and medical interventions used to manage and alleviate the symptoms of diverticulosis. Patients should note the role of regular monitoring and lifestyle adjustments in effectively managing this condition.
- Dietary Changes: The primary focus in managing diverticulosis is to prevent the formation of new diverticula and reduce the risk of complications. Increasing dietary fibre intake is key to softening the stool and preventing constipation, which can help lower pressure in the colon. This can be achieved by consuming more fruits, vegetables, whole grains, and legumes.
- Hydration: Drinking plenty of fluids, especially water, helps maintain regular bowel movements and prevent constipation.
- Lifestyle Modifications: Maintaining a healthy lifestyle that includes regular physical activity and avoiding smoking can also help reduce the risk of diverticular disease.
Diverticulitis Treatments
A number of treatments for diverticulitis are available ranging from antibiotics and dietary modifications for mild cases to potential surgical interventions for severe or recurrent episodes. The focus is on personalised treatment plans that address the severity and frequency of symptoms to ensure optimal patient outcomes.
- Antibiotics: In cases of mild diverticulitis, where there are minimal symptoms and no signs of complications, antibiotics may be prescribed to treat the infection and reduce inflammation.
- Clear Liquid Diet: During an acute episode of diverticulitis, a clear liquid diet may be recommended for a few days to rest the digestive system. This can include broth, clear soups, gelatin, and clear juices.
- Low-Fibre Diet Transition: After the initial phase of clear liquids, a low-fibre diet may be introduced to allow the colon to heal. This diet typically includes foods like white rice, white bread, pasta, and canned fruits.
- Gradual Return to Regular Diet: Once the acute symptoms improve, a gradual transition to a high-fibre diet is encouraged to prevent future episodes of diverticulitis. This can include reintroducing fibre-rich foods like fruits, vegetables, and whole grains.
- Pain Management: Over-the-counter pain relievers or prescription medications may be used to manage abdominal pain and discomfort.
- Hospitalisation: Severe cases of diverticulitis with complications such as abscesses, bowel obstruction, or peritonitis may require hospitalisation and intravenous antibiotics. In some instances, drainage of abscesses or surgical intervention may be necessary.
- Surgery: Diverticulitis surgery is typically reserved for recurrent, severe, or complicated cases, where other treatments have not been effective. It usually involves removing the affected section of your large intestine, called a colectomy. This is the treatment for rare complications such as fistulas, peritonitis or a blockage in your intestines.The most common complication of diverticulitis is developing abscesses. Severe abscesses are drained with a technique known as percutaneous drainage, which is done by a radiologist. Often, after the abscess is successfully drained, surgery can be planned electively.
How Is Diverticular Disease Diagnosed
Diagnosing diverticular disease typically involves a combination of medical history evaluation, physical examination, and various diagnostic tests. The specific tests and procedures used may vary depending on whether the focus is on diverticulosis (presence of diverticula without inflammation) or diverticulitis (inflammation or infection of diverticula).
Here are common methods for diagnosing diverticular disease:
Medical History And Physical Examination
Your healthcare provider will start by taking a detailed medical history, including information about your symptoms, their duration, and any previous episodes. A physical examination may be performed to check for tenderness or abdominal pain, which is common in diverticulitis.
Blood Tests
Blood tests, including a complete blood count (CBC), may be conducted to check for signs of infection or inflammation, such as an elevated white blood cell count.
Imaging Studies
Imaging tests are crucial for diagnosing and evaluating diverticular disease. These tools make it easier for healthcare providers to accurately identify diverticular disease and help in deciding on the best treatment options:
- Computed Tomography (CT) Scan: CT scans of the abdomen and pelvis are commonly used to visualise the colon and detect the presence of diverticula and any complications, such as abscesses or perforations.
- Barium Enema: This is a contrast study where barium sulphate is used to outline the colon’s shape and detect any abnormalities, including diverticula. However, it is less commonly used today, with CT scans being preferred.
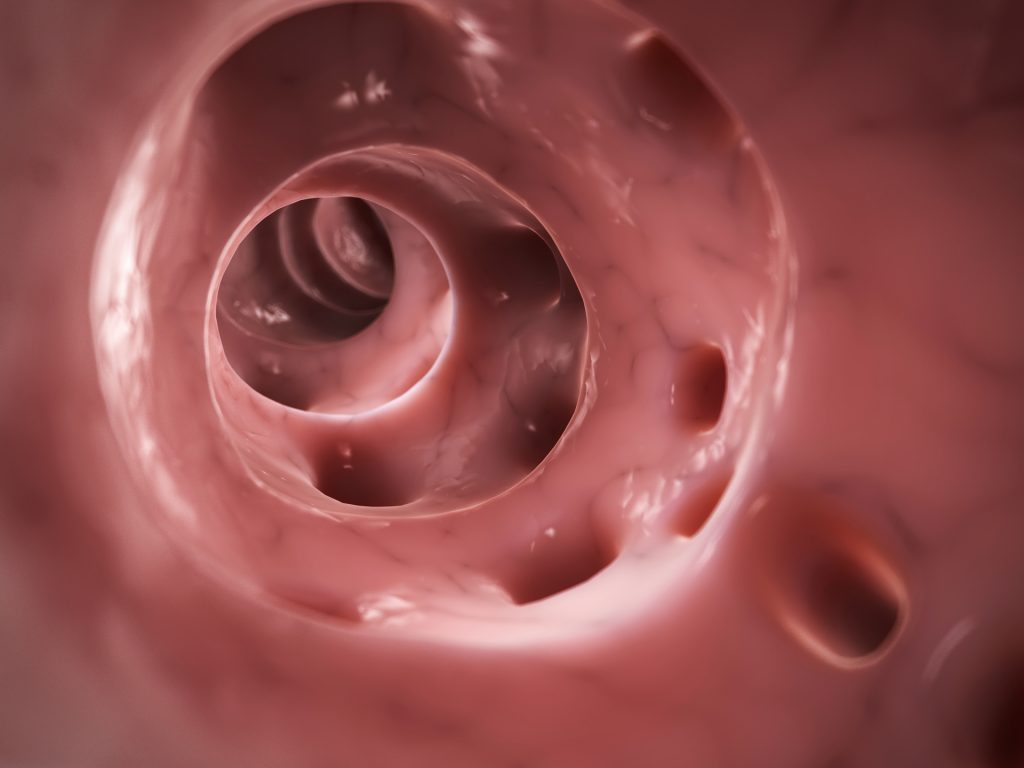
Colonoscopy
A colonoscopy is an endoscopic procedure in which a flexible tube with a camera is inserted into the rectum and advanced through the colon. It allows direct visualisation of the colon’s interior and can detect diverticula, rule out other conditions, and help evaluate the overall health of the colon.
How We Can Help With Diverticular Disease In Singapore
Dr QM Leong is an experienced colorectal doctor with relevant medical specialities in laparoscopic surgery, colorectal surgery, diverticular disease treatment and will accurately diagnose your condition for any signs or common symptoms before determining the ideal treatment to prevent diverticular disease for your condition.
We are fully committed to providing a pleasant experience, treatment and patient care, so do not hesitate to seek immediate medication attention by calling us to find out about diverticulitis or make an appointment with us to understand more about it.
Frequently Asked Questions About Diverticular Disease In Singapore
Is Diverticular Disease In Singapore Serious?
Is Diverticular Disease Common In Singapore?
Should I Worry About Diverticular Disease?
About Dr QM Leong
Colorectal & Hernia Surgeon in Singapore
Dr Leong is a general and colorectal surgeon in Singapore who graduated from the University of London in 2000. He obtained his membership to the Royal College of Surgeons of Edinburgh in 2003 and started working in Tan Tock Seng Hospital in 2003. He started his Advanced Specialist Training in 2005 and passed his fellowship exams in 2008. Dr Leong was awarded the prestigious MOH HMDP scholarship to train under Prof Kim Seon Hahn in Korea University for Laparoscopic and Robotic colorectal surgery in 2010.
Dr Leong is amongst a handful of hernia and colorectal surgeons in Singapore who practice Single Incision Laparoscopic surgery. This is a technical and complex procedure that is minimally invasive, speeds up recovery, and confers excellent cosmetic results. Dr Leong also routinely trains basic and advanced specialist trainees in laparoscopic surgery, and regularly proctors consultant surgeons in complex colorectal cases.
Beyond laparoscopic surgery, Dr Leong also performs a repertoire of minimally invasive General Surgery procedures. He is also an experienced endoscopist with more than 10000 procedures, performing diagnostic and therapeutic scopes for elective and emergency surgical conditions. He performs direct access colonoscopies and oesophago-gastro-duodenoscopy for patients and will strive to perform the procedures on the same day if possible for patients’ convenience.

Insurance
Our surgery is on the panel of most of the major insurance companies and if you are covered by corporate insurance, you may be entitled to a cashless visit to our clinic.
Get In Touch
Corporate Insurance Partners











Personal Insurance Partners







